In the rapidly evolving world of healthcare technology, EHR integration stands at the forefront of innovation. It’s the vital link connecting patient care, cutting-edge technology, and efficient healthcare management. When custom healthcare products successfully integrate with EHR systems, we see streamlined workflows, improved patient care, and data-driven decision-making becoming the norm rather than the exception.
However, let’s be honest – integrating EHR into custom healthcare products isn’t a walk in the park. It comes with its own set of challenges and requires careful planning, technical expertise, and a keen eye for compliance. But don’t worry, we’re here to guide you through the process.
In this comprehensive guide, we’ll explore:
- The ins and outs of EHR integration
- Common hurdles you might face (and how to overcome them)
- The game-changing benefits of successful integration
- A step-by-step approach to implementation
- Best practices and future trends in EHR integration
Let’s go!
Understanding EHR Systems and Integration
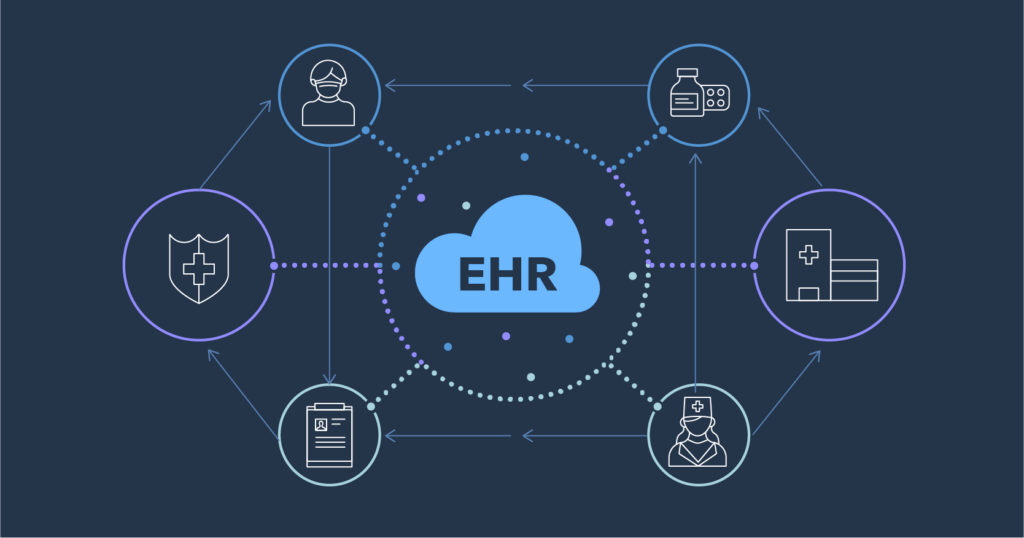
Electronic Health Records (EHR) have revolutionized the healthcare landscape by digitizing patient information and making it readily accessible to healthcare providers. These systems are the digital file cabinets of the medical world, storing everything from a patient’s medical history and diagnoses to medications, treatment plans, immunization dates, and test results – all in a secure, electronic format.
But EHR integration? That’s where the magic really happens. It’s about creating a seamless connection between multiple healthcare technologies. Think of it as teaching all your different medical systems to speak the same language fluently. When we talk about EHR integration, we’re referring to the process of connecting EHRs with other digital systems like laboratory information systems (LIS), pharmacy management systems, and various medical devices.
The result? Real-time healthcare data exchange that reduces errors, eliminates redundant data entry, and ultimately leads to better patient care. It’s like upgrading from a relay race of information to a synchronized dance of data.
Challenges in EHR Integration: It's Not All Rainbows and Unicorns
Now, before you go thinking EHR integration is a walk in the park, let’s talk about the elephant in the room – or should I say, the dinosaurs in the server room. Here are the hurdles that’ll make you want to pull your hair out (if you haven’t already from dealing with insurance companies):
System compatibility
Imagine trying to get your great-aunt’s Windows 95 computer to chat with your swanky new MacBook. That’s the kind of headache we’re dealing with here. Many healthcare orgs are running on systems older than your favorite dad jokes, and they’re about as compatible with new tech as oil is with water.
What happens when these old-timers meet new tech? It’s not pretty:
- Data gets stuck in silos tighter than your jeans after Thanksgiving dinner.
- You end up spending more money.
- The time it takes to upgrade? Let’s just say you could probably binge-watch all seasons of Grey’s Anatomy. Twice.
But don’t worry! At Cadabra Studio, we’re like tech whisperers for these cranky old systems. We’ve got more integration tricks up our sleeves than a magician at a medical conference.
2. Data security and HIPAA compliance
When it comes to EHR systems, data security isn’t just important – it’s paramount. Patient data is sensitive, and its protection is governed by strict regulations like HIPAA. Key concerns include:
- Data breaches: Healthcare data is a prime target for cyberattacks due to its comprehensive nature, including personal and financial information.
- Regulatory compliance: Strict guidelines dictate how patient data should be stored, transmitted, and accessed. Any integration must ensure data is protected at all points without compromising usability.
- User permissions: Managing access rights across multiple systems can be complex, especially with custom solutions.
A single misstep in securing patient data can lead to severe legal consequences and irreparable damage to an organization’s reputation.
3. User adoption
Even the most advanced EHR systems can fail if healthcare professionals struggle to use them effectively. User adoption is a significant hurdle, often stemming from:
- Steep learning curves: Healthcare professionals are often pressed for time, and learning a new system can feel like an additional burden.
- Resistance to change: Many healthcare workers are accustomed to their existing workflows, and new technology can disrupt these familiar routines.
- Integration with existing workflows: The success of an integration project depends not just on technical compatibility but on how well the new system fits into existing clinical processes.
The key to overcoming this challenge lies in proper training, ongoing support, and designing systems that align closely with how healthcare professionals actually work.
Benefits of Successful EHR Integration
When done right, EHR integration can transform healthcare operations, enhancing both efficiency and patient care. Let’s explore the key benefits:
Streamlined Workflows
In the fast-paced world of healthcare, time is a precious commodity. EHR integration helps alleviate time pressures by centralizing patient data. When all relevant health information is accessible in one system, healthcare professionals can:
- Significantly reduce manual data entry
- Improve team coordination
- Automate administrative tasks like appointment scheduling and billing
- Minimize the risk of human error
For healthcare organizations, this translates to faster workflows, better resource utilization, and more time dedicated to patient care rather than paperwork.
2. Data-Driven Care
Integrated EHR systems empower healthcare professionals with comprehensive, real-time patient information at the point of care. This includes:
- Comprehensive patient histories: Access to past surgeries, allergies, current treatments, and family medical history enables more informed decision-making.
- Real-time updates: The latest lab results, diagnostic reports, or medication changes are immediately available, allowing for swift adjustments to care plans.
- Predictive insights: Advanced EHR systems with analytics capabilities can use historical data to predict health outcomes, enabling proactive care and risk management.
This wealth of information facilitates a more holistic approach to patient care, reducing the likelihood of misdiagnosis and treatment delays.
3. Enhanced Patient Experience
EHR integration significantly improves the patient experience in several ways:
- More face time with providers: With integrated systems, physicians spend less time searching for information and more time interacting with patients.
- Patient engagement: Many EHR systems include patient portals where individuals can access their medical records, fostering greater engagement in personal healthcare.
- Reduced redundancy: With full access to a patient’s medical history, providers can avoid duplicate tests or procedures, saving time, money, and patient discomfort.
- Continuity of care: As patients move between care settings, their complete medical records follow, ensuring smooth transitions and consistent care.
By streamlining processes and improving access to information, EHR integration contributes to a healthcare experience that’s more efficient, personalized, and patient-centric.
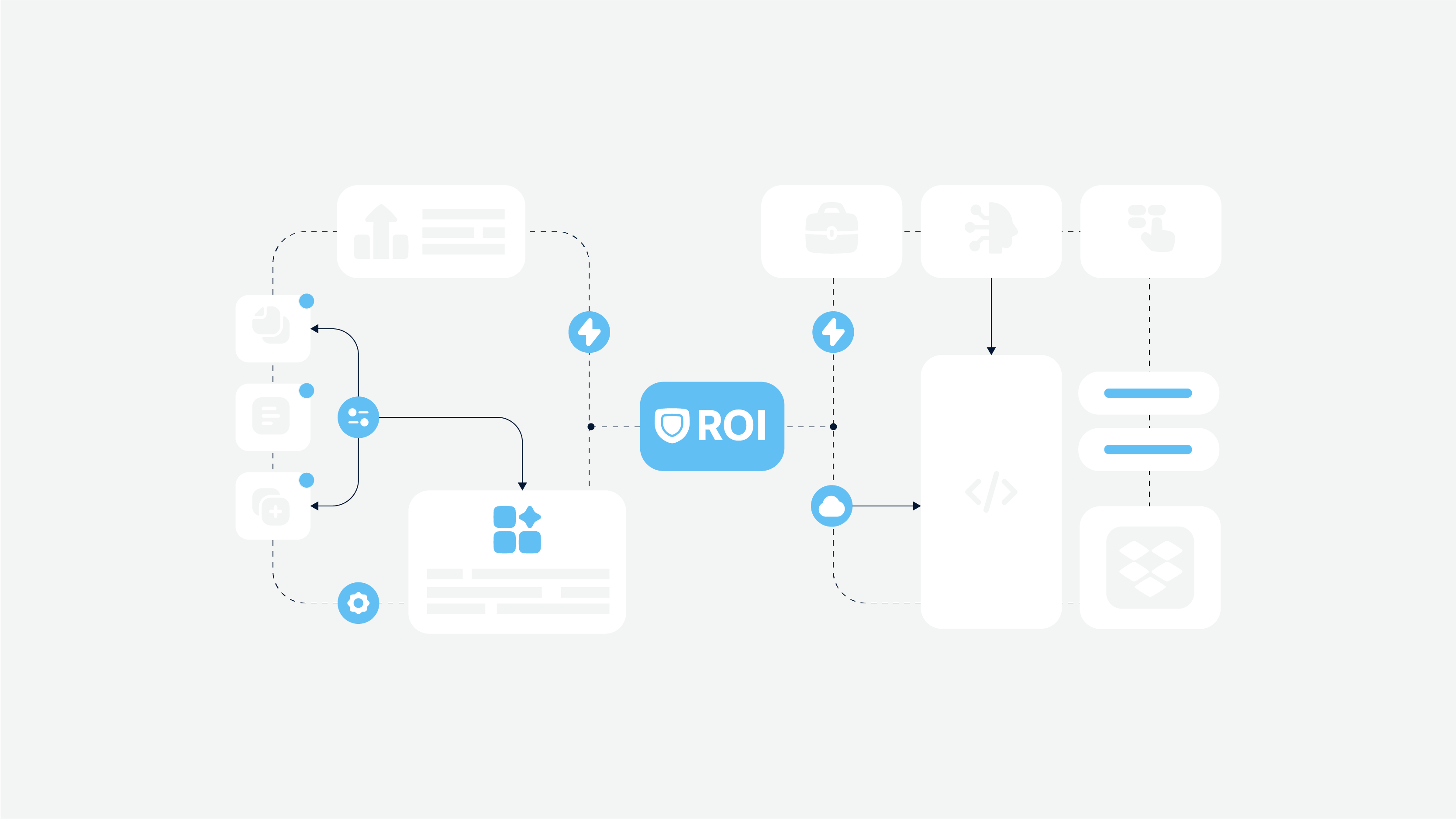
EHR Integration Step-by-Step Guide: Your Treasure Map to Healthcare Harmony
Disclaimer: This guide is as simplified as a kid’s connect-the-dots puzzle. Why? Because every healthcare org is as unique as a snowflake in a blizzard. But fear not! If you need a plan tailored just for you, give us a shout. We’re like the Fairy Godmothers of EHR integration, minus the magic wand (we use keyboards instead).
While every healthcare organization has unique needs, here’s a general roadmap for EHR integration:
1. Asses current systems
Begin by taking a comprehensive inventory of your existing IT infrastructure:
- Identify all systems currently in use
- Evaluate their compatibility with EHR integration
- Understand current workflows to plan integration without disrupting care
2. Define integration goals and requirements
Clarity is key in this stage:
- Specify data exchange requirements (e.g., lab results, prescriptions, patient histories)
- Outline use cases (routine check-ups, emergency care, chronic disease management)
- Map out how other systems (billing, pharmacy) will interact with the EHR
3. Choose the right integration framework
Selecting appropriate integration standards is crucial for seamless data exchange:
- Consider standards like HL7 (Health Level 7) or FHIR (Fast Healthcare Interoperability Resources)
- FHIR is gaining popularity due to its ability to handle complex data sets and its flexibility with different types of healthcare software
4. Think about security. Always.
Given the sensitive nature of healthcare data, security should be a top priority:
- Implement robust encryption for data in transit and at rest
- Establish role-based access controls (RBAC)
- Set up comprehensive audit trails to monitor data access
5. Test and validate
Before going live, thorough testing is essential:
- Conduct functional testing to ensure the system works as expected
- Perform security testing to verify data protection measures
Remember, while this guide provides a solid foundation, each integration project will have its unique challenges and requirements. At Cadabra Studio, we specialize in tailoring the integration process to meet the specific needs of each healthcare organization we work with.
FHIR Standards and Healthcare Interoperability
As the healthcare industry evolves, the need for seamless data exchange becomes increasingly critical. This is where FHIR (Fast Healthcare Interoperability Resources) comes into play, revolutionizing healthcare interoperability.
How FHIR works
FHIR breaks down healthcare data into standardized “resources” – small, modular components that represent specific parts of healthcare information. These may be patient demographics, lab results, or prescriptions.
These resources are customizable, so they can be adapted to the needs of different systems with healthcare interoperability. FHIR also supports RESTful APIs, which allow real-time, scalable data exchange over the web using simple, widely used technologies like HTTP.
A modular and customizable structure is the reason why FHIR has been adopted by the healthcare community, especially for integrationg EHR in custom healthcare software.
Understanding FHIR
FHIR is a next-generation standards framework created by HL7. It combines the best features of HL7’s v2, v3, and CDA product lines while leveraging the latest web standards and applying a tight focus on implementability.
Key Features of FHIR:
- Modular Components: FHIR breaks down healthcare data into standardized “resources” – small, discrete units of information that can be easily combined or modified.
- RESTful API: FHIR leverages modern web technologies, making it easier to implement and more accessible for developers.
- Human Readability: Unlike some previous standards, FHIR resources are designed to be understandable by both machines and humans.
Why FHIR Matters for EHR Integration
- Enhanced Interoperability: FHIR enables different healthcare systems to communicate more effectively, reducing data silos and improving care coordination.
- Flexibility: The modular nature of FHIR allows for easy customization and adaptation to various healthcare scenarios.
- Cost-Effective Implementation: By using widely adopted web standards, FHIR can often be implemented more quickly and at a lower cost than previous standards.
- Future-Proofing: As healthcare needs evolve, FHIR’s flexible structure allows for easier updates and additions to the system.
Real-World Impact of FHIR
- Improved Patient Care: With faster, more comprehensive data exchange, healthcare providers can make more informed decisions.
- Enhanced Patient Engagement: FHIR facilitates the development of patient-facing apps that can easily integrate with provider systems.
- Research Advancements: The standardized format of FHIR data makes it easier to aggregate and analyze large datasets for medical research.
While FHIR represents a significant advancement in healthcare interoperability, it’s important to note that its implementation requires careful planning and expertise. At Cadabra Studio, we’ve successfully integrated FHIR-based solutions into numerous healthcare systems, helping our clients stay at the forefront of healthcare technology.
Case Study: How We Turned a Health Portal from Meh to Marvelous
We’re about to spill the beans on how we transformed a clunky health portal into a lean, mean, patient-pleasing machine.
Background
A healthcare provider specializing in chronic disease management approached us with a challenge. They needed a custom patient health portal that would:
- Improve care coordination
- Provide patients with easy access to their medical records
- Allow patients to track health metrics and communicate with their care team
- Enhance medical data integration and patient data management
Challenges
- The existing patient management system was not user-friendly and had limited patient engagement features.
- Data integration from multiple sources (labs, prescriptions, wearables) was complex.
- The platform needed to be fully HIPAA compliant.
Solution
We rolled up our sleeves and got to work faster than a cat video goes viral. We built a custom health portal. Here’s how we sprinkled our magic:
- FHIR Power: We harnessed the power of FHIR standards, making data flow smoother than a well-oiled slip ‘n slide.
- Security Fort Knox: We locked that data down tighter than your grandma’s secret cookie recipe.
- User Experience Elevation: We made the interface so intuitive, even your tech-phobic uncle could navigate it.
Using the right framework for healthcare software development, we could kill two birds with one stone: ensure rich functionality and meet strict HIPAA standards.
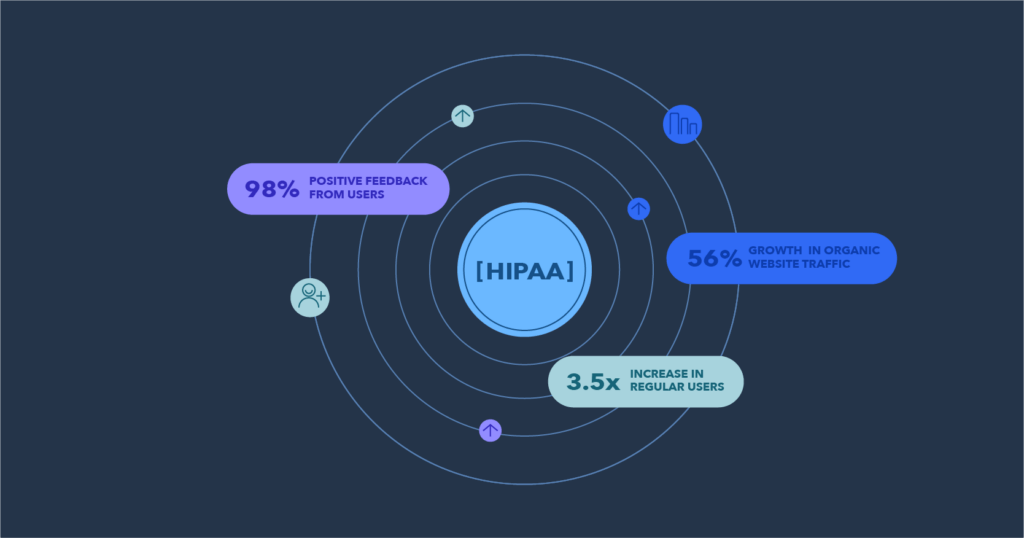
Results
The impact of the new system was significant:
- – 3.5x increase in regular users
- – 56% growth in organic website traffic
- – 98% positive feedback from users
- – Streamlined content management and improved reporting functionality
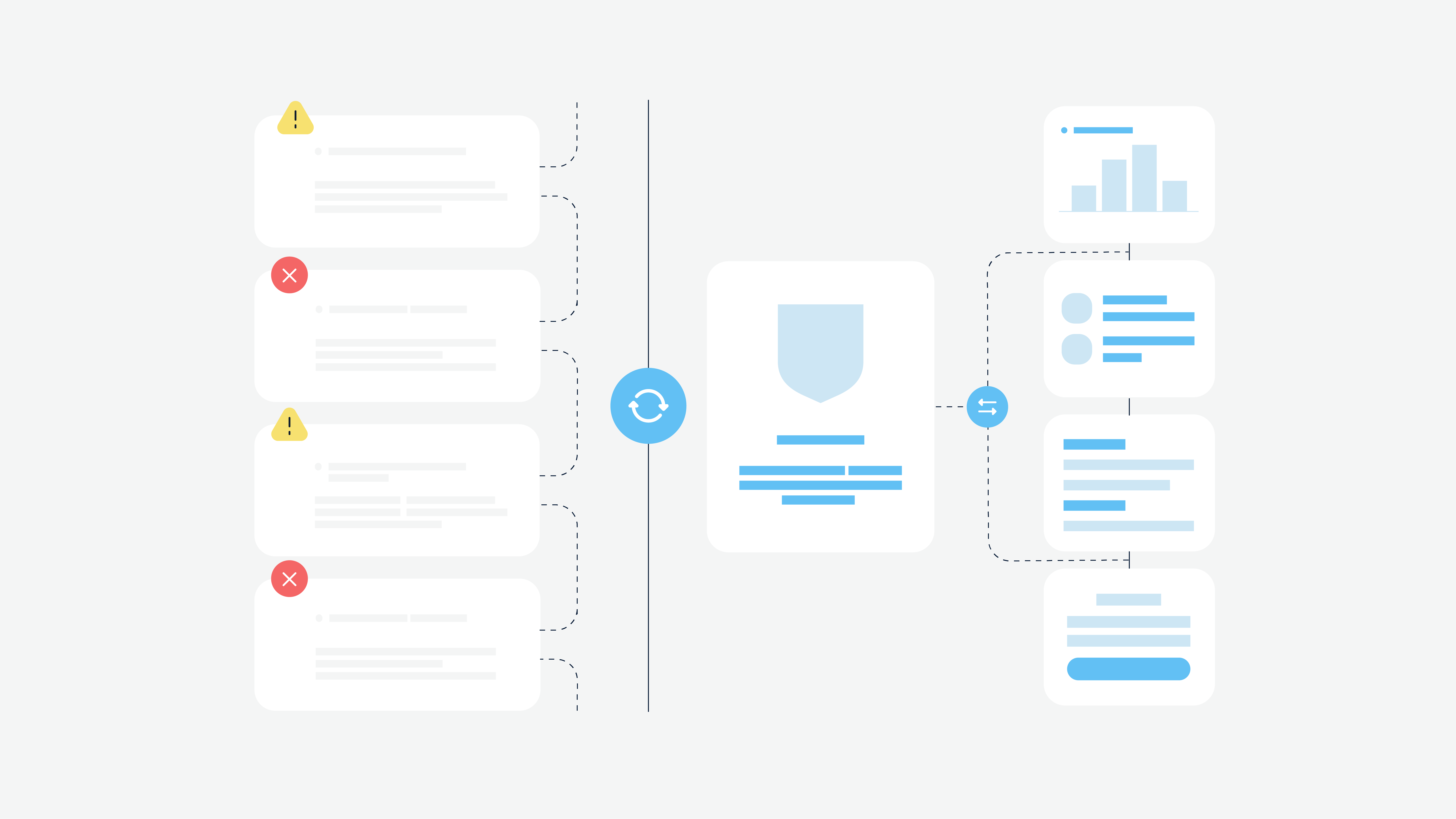
HIPAA Compliance and Data Security: Safeguarding Patient Information
Integrating EHR systems into custom healthcare software requires strict compliance with HIPAA (Health Insurance Portability and Accountability Act) regulations. Okay, maybe HIPAA compliance isn’t as thrilling as a medical drama season finale, but in the world of healthcare IT, it’s more critical than caffeinated nightshift nurses.
In EHR data security is even more critical as healthcare providers are managing more patient data across multiple systems. Here are some key security measures to comply with.
Data encryption
HIPAA requires all patient data, whether at rest (stored in a database) or in transit (being transmitted between systems) to be encrypted to protect it from unauthorized access. Encryption ensures that even if data is intercepted or accessed illegally it remains unreadable and secure.
Encryption algorithms should meet the latest industry standards so healthcare providers and developers comply with HIPAA’s Security Rule.
- At-rest encryption – encrypting patient data stored on servers, databases, or any local device to prevent unauthorized access in case of a breach.
- In-transit encryption – using Secure Socket Layer (SSL) or Transport Layer Security (TLS) protocols to protect data as it moves between systems, e.g., during communication between an EHR system and custom healthcare software.
Access control
Role-based access control (RBAC) ensures that only authorized individuals – doctors, nurses, or administrative staff – have access to specific patient data relevant to their role. This reduces the risk of exposing sensitive information to those who don’t need it.
Here are HIPAA’s key access controls:
- multi-factor authentication (MFA);
- role-based permissions;
- session timeouts.
Audit trails
HIPAA also requires healthcare organizations to maintain audit trails – detailed logs that record every instance of data access, modification, and transfer. These logs track which user accessed what patient information, when and what actions were performed.
By reviewing audit logs, healthcare organizations can detect suspicious activity, e.g., an employee accessing data outside their job role or unusual access times. In case of a data breach or other security incident audit trails provide a record that can be used to identify the source of the breach and determine the extent of the damage.
EHR Integration Best Practices
Now, let’s discuss how to make your EHR integration as smooth and effective as possible:
1. User-Centric Design
Remember, your end-users are juggling patients, paperwork, and probably a caffeine addiction. Make their lives easier:
- Simplify the interface. Make the system easy to use and intuitive, and reduce the learning curve for healthcare staff.
- Focus on workflows. Don’t overload users with unnecessary steps. Design the interface to mirror healthcare providers’ existing workflows to encourage adoption and make it easier to slot into daily routines.
- Provide training. Offering comprehensive training sessions and ongoing support for healthcare professionals will help with the transition to new systems and build user confidence.
2. Interoperability
Your EHR system should be friendlier than a golden retriever at a dog park:
- Embrace standards like FHIR: It’s the cool kid in the interoperability schoolyard.
- Future-proof your system: Because nobody wants to do this all over again in five years.
3. Ongoing support
EHR system isn’t the finish line; it’s just the starting gun:
- Regular check-ins: Be more persistent than a toddler asking “why?”
- Stay updated: Keep your system fresher than the produce section.
- Listen to feedback: Your users aren’t just pretty faces in scrubs. They’ve got valuable insights!
Pro Tip: Regularly gathering feedback is like giving your EHR system a health check-up. It keeps it fit, agile, and ready to meet your users’ needs.
Future Trends in EHR Integration
AI and Machine Learning
Artificial intelligence (AI) and machine learning (ML) have already revolutionized EHR systems. But they continue to evolve and create new bright opportunities for the medical field.
Here are some of the most prominent trends is using AI and ML:
- Predict patient outcomes (AI can analyze data in seconds and predict patient complications or readmissions, so they can intervene earlier)
- Personalise treatment plans (Machine learning algorithms can analyze patient data to identify patterns that inform personalized care plans, tailored to the individual patient)
- Decision support (AI-powered tools can provide real-time clinical decision support by offering recommendations based on the latest medical research and a patient’s health history)
Mobile-first EHR solutions
Mobile-first EHR solutions are the only way to keep users attention. In the case of healthcare, providers can access patient records on the go, whether in a hospital, at home, or in remote areas.
Mobile apps can allow patients to monitor their health, book appointments, and communicate with their healthcare providers more easily. And patients’ devices can collect real-time data from wearables, giving healthcare professionals a fuller picture of a patient’s health.
Blockchain for data exchange
Blockchain is highly used in the fintech sector for its ability to secure data and improve data traceability. For EHR, blockchain will also be very beneficial.
Firstly, its decentralized nature means once data is recorded, it can’t be changed without being detected, so patient records are secure. The transparent ledger for all transactions involving patient data blockchain can reduce the risk of tampering or unauthorized access.
Secondly, it can give patients more control over their medical records and grant or revoke access to their data as needed
Conclusion: Embracing the Future of Healthcare Technology
EHR integration is more than just a technological upgrade – it’s a fundamental shift in how healthcare is delivered and experienced. As we’ve explored in this guide, successful integration can streamline workflows, improve patient care, and drive data-driven decision-making in healthcare organizations.
Key Takeaways:
- EHR integration, while challenging, offers significant benefits in terms of efficiency, patient care, and data management.
- Overcoming integration challenges requires a strategic approach, focusing on system compatibility, data security, and user adoption.
- FHIR standards are playing a crucial role in advancing healthcare interoperability.
- HIPAA compliance and robust data security measures are non-negotiable in EHR integration.
- The future of EHR systems lies in AI integration, mobile solutions, and enhanced interoperability.
At Cadabra Studio, we’re committed to helping healthcare organizations navigate the complexities of EHR integration. Our expertise in custom healthcare software development, combined with our deep understanding of healthcare regulations and best practices, positions us to deliver solutions that not only meet current needs but are also prepared for future advancements.
As you consider your own EHR integration journey, remember that the goal is not just to implement new technology, but to transform your healthcare delivery for the better. With the right approach and partner, EHR integration can be a powerful tool in improving patient outcomes, enhancing operational efficiency, and positioning your organization at the forefront of healthcare innovation.
Ready to take the next step in your EHR integration journey? Contact Cadabra Studio today. Let’s work together to create a healthcare future that’s more connected, efficient, and patient-centered than ever before.