Medical software development has come a long way from clunky, disconnected systems to the sophisticated, AI-powered platforms we see today. As we move deeper into 2025, the industry faces a paradox: immense technological advancements paired with increasing complexity.
As a healthcare software development company, we understand that, innovation promises better patient outcomes and streamlined operations. However, healthcare managers and software implementers still grapple with integration headaches, compliance mazes, and user adoption struggles.
In this guide, I’ll break down the modern world of software development healthcare and offer practical insights into challenges. I’ll also share healthcare software examples, best practices, and future trends.
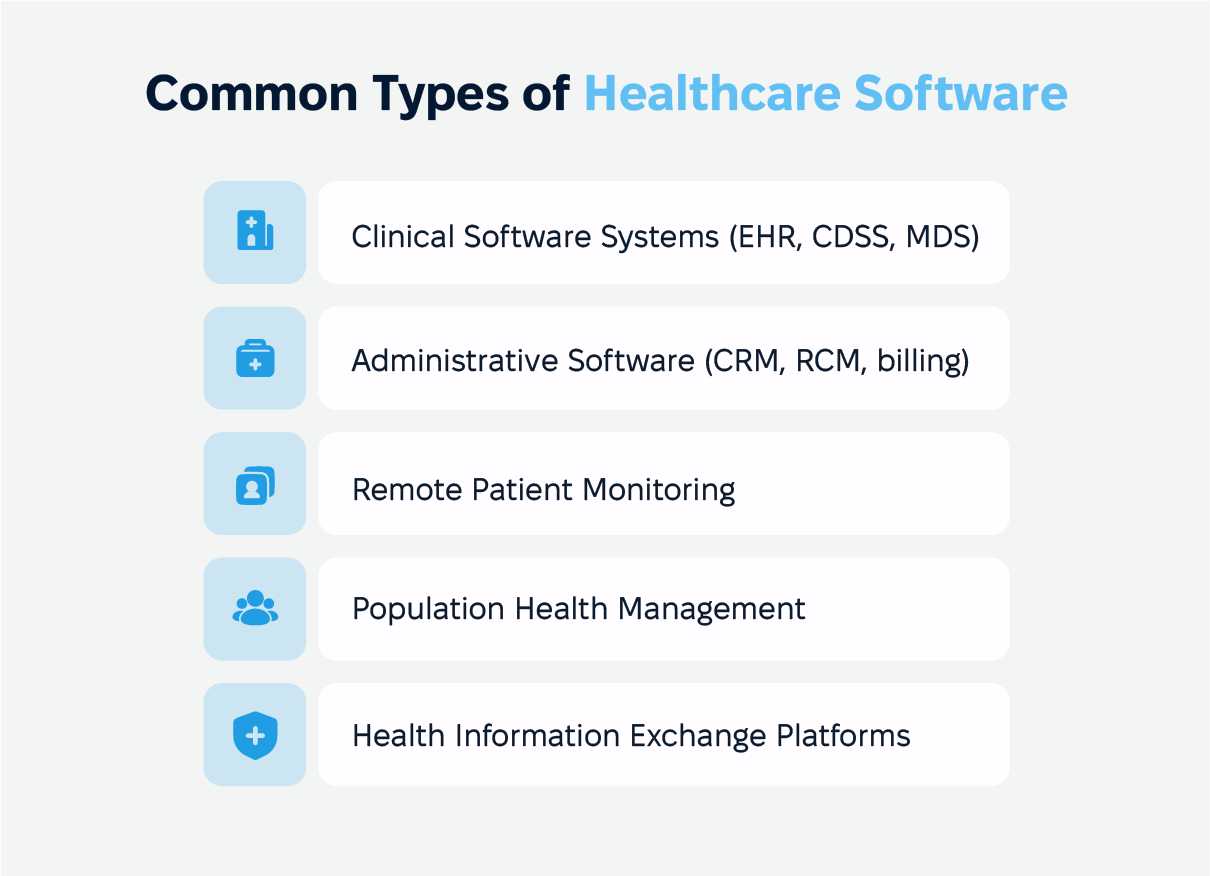
5 Main Types of Healthcare Software
Here’s a striking reality: A study by McKinsey found that companies with strong digital capabilities outperform their peers by up to 50% in terms of revenue growth. In healthcare, where medical software plays a direct role in patient care and operational efficiency, falling behind on technology isn’t just an inconvenience—it can mean the difference between life and death.
As we explore the latest trends and strategies, keep in mind: the right digital solution for medical professionals is the purest and the strongest competitive advantage that defines the future of healthcare. And here are the 5 different types of software used in healthcare industry you should pay attention to.
Clinical Software Systems
At the heart of modern healthcare are clinical software solutions that enhance patient care and provider decision-making. Electronic Health Records software (EHR) remain foundational, evolving with improved interoperability and AI-powered data insights.
Clinical Decision Support Systems (CDSS) or Medical Diagnosis Software help providers make evidence-based decisions by analyzing vast amounts of medical data in real time. Telemedicine platforms, once an emerging trend, are now indispensable, offering virtual consultations, remote patient monitoring, and AI-driven diagnostics that bring healthcare to patients wherever they are.
Administrative Software
Beyond clinical care, healthcare organizations rely on administrative software to keep operations running smoothly. Healthcare Customer Relationship Management (CRM) systems enhance patient engagement, automating appointment reminders and follow-ups to reduce no-show rates. CRM software for healthcare simplifies scheduling, billing, and documentation, reducing administrative burdens.
Revenue Cycle Management (RCM) platforms ensure accurate claims processing and reimbursement tracking, helping healthcare providers maintain financial stability in an increasingly complex reimbursement landscape. More examples are medical equipment management software and medical billing software.
Remote Patient Monitoring (RPM)
Keeping an eye on patients beyond the walls of a hospital or clinic used to be nearly impossible, but Remote Patient Monitoring (RPM) is changing that. Using devices like smartwatches, blood pressure cuffs, and glucose monitors, doctors can now track a patient’s health from miles away.
This means fewer unnecessary trips to the hospital, earlier detection of potential health issues, and better management of chronic conditions like diabetes and heart disease. For patients, it’s peace of mind knowing their health is being monitored without disrupting their daily lives.
Population Health Management (PHM) Platforms
Managing healthcare services for large groups of people isn’t just about treating individuals—it’s about spotting patterns and preventing problems before they escalate. Population Health Management (PHM) platforms gather information from electronic health records, insurance claims, and even wearable devices to help healthcare organizations see the bigger picture.
By analyzing trends, they can predict which communities are at risk for certain illnesses and take action early, like rolling out targeted screenings or wellness programs. It’s like having a crystal ball for public health, helping providers make smarter decisions that improve care for entire populations.
Health Information Exchange (HIE) Platforms
Imagine if every time you saw a new doctor, you had to start from scratch—repeating your entire medical history, getting the same tests done over and over. That’s what happens when healthcare systems don’t talk to each other. Health Information Exchange (HIE) platforms fix this by securely sharing patient records between hospitals, clinics, and specialists.
This means no more redundant tests, fewer medical errors, and smoother transitions between different providers. Whether a patient moves to a new city or just switches doctors, their medical history follows them, ensuring they get the best possible care without the usual roadblocks.
There are many more examples of custom healthcare solutions. Contact us to discuss the one you need
Key Requirements for Healthcare Software Development
Healthcare software needs to run smoothly and keep patient data safe so that both care and privacy are taken care of properly. The healthcare industry has a lot of moving parts, so the software must meet key requirements to be dependable and flexible enough to keep up with changing needs.
Healthcare Software Compliance and Security
In healthcare, software must follow strict rules about how patient data is collected, stored, and used. These regulatory compliance standards, like HIPAA and GDPR, help protect patients’ personal information. To keep data safe, software should use encryption, ensure only authorized people can access it, and conduct regular security checks. With the rise of cyber threats, security measures must always be updated and ahead of the curve.
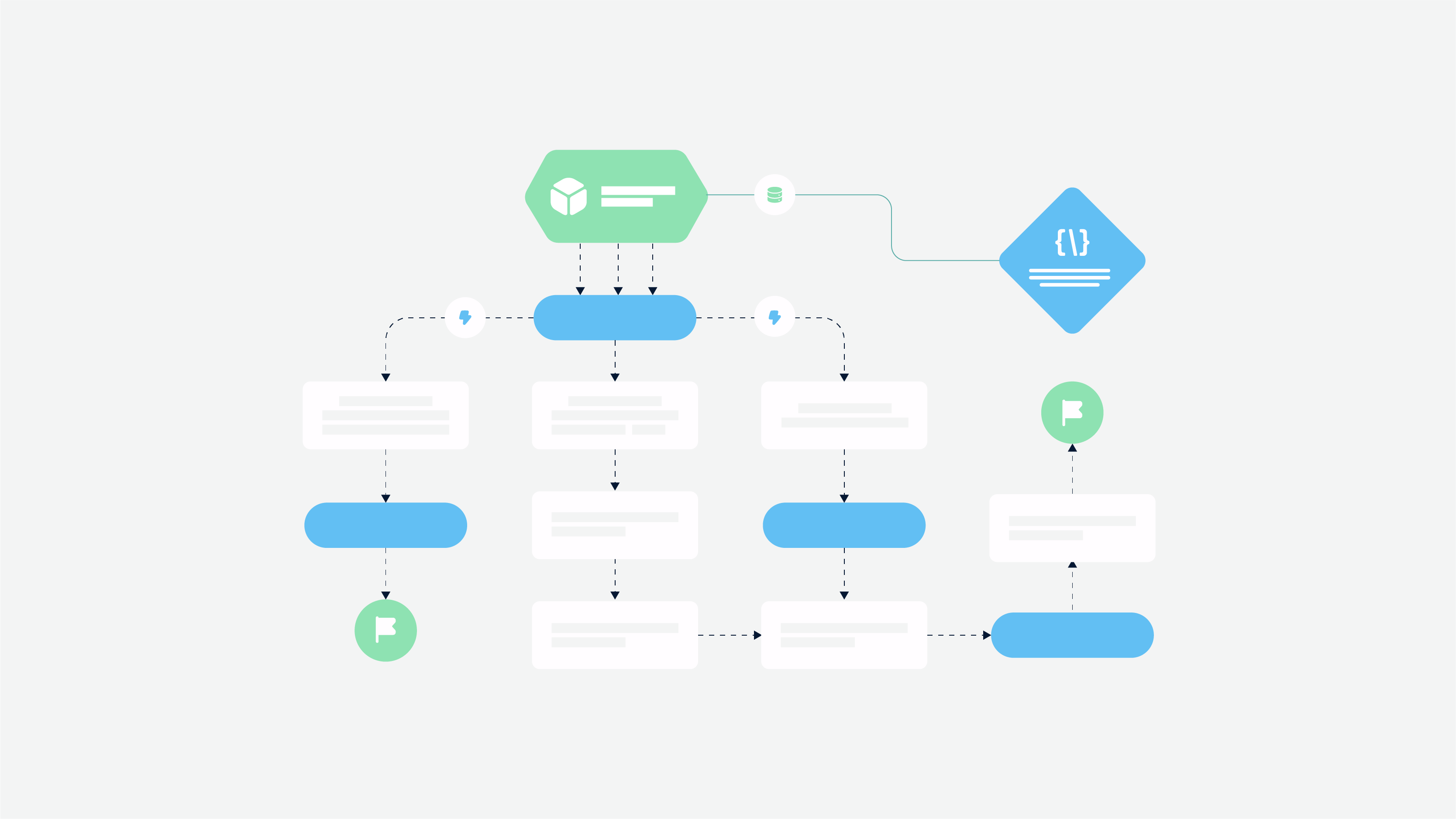
Integration Capabilities
Healthcare systems work best when they can exchange information easily. However, many older systems don’t connect well with newer ones. Software needs to support smooth healthcare software integration with other tools, such as lab systems, pharmacies, and insurance platforms.
This way, everyone involved in a patient’s care can access accurate data when needed. Good integration reduces disruptions and ensures that all systems work together without errors.
Scalability and Flexibility
As healthcare needs grow, so do the demands on software. Systems need to be flexible enough to handle more patients and larger amounts of data. Cloud technology offers a simple solution, allowing healthcare organizations to increase their resources as needed.
According to a 2024 survey by HIMSS, 60% of healthcare organizations plan to use more cloud computing in the coming year to handle data growth and improve efficiency.
User Experience (UX) and Accessibility
The success of healthcare software often comes down to how easy it is to use. Systems that are simple to navigate help healthcare workers and patients alike. A well-designed interface means less time spent on training and fewer mistakes.
A 2025 study by the Journal of Medical Internet Research showed that healthcare systems with clear designs cut training time by 30%, making tasks quicker and more efficient.
Data Analytics and Reporting
Data is valuable, but only when it can be used to improve care. Healthcare software should include tools that turn data into useful insights.
For example, it can predict which patients are at risk of being readmitted to the hospital or help make staffing decisions. A 2024 report by Gartner found that 72% of healthcare providers are already using analytics to improve patient care and cut costs.
Healthcare Software Development Challenges
Creating healthcare software comes with its own set of challenges. While it’s an exciting field with tons of potential, developers face a few key hurdles that can make the process tough. Let’s take a look at the biggest ones.
User Adoption Barriers
Getting healthcare professionals to actually use new software can be tricky. Many are comfortable with the systems they already know, and switching to something new can feel like a hassle.
The software has to be easy to use, and it has to show clear benefits for everyday tasks. If it feels like it’s making their job easier, users are much more likely to adopt it. But if it’s complicated or feels unnecessary, they might resist.
Legacy System Integration
Many healthcare organizations still rely on older systems, and getting new software to play nicely with these legacy tools is a big challenge. Whether it’s patient records or billing software, old systems can be tough to integrate with new technology.
Developers have to find ways to make sure everything works together smoothly without causing any disruptions. It takes time and careful planning, but it’s essential for making sure no data gets lost, and everything keeps running as it should.
Compliance Complexities
Healthcare is one of the most regulated industries, and making sure software meets all the legal requirements is no small task. Whether it’s HIPAA in the U.S. or GDPR in Europe, developers have to stay on top of ever-changing laws about patient data.
This means the software needs strong security measures, like encryption and secure logins, to protect sensitive information. Compliance adds extra complexity, but it’s necessary to keep everything secure and trustworthy.
Stakeholder Management
Building software for healthcare means dealing with a lot of different people with different needs. Doctors, nurses, patients, hospital administrators, and even regulators all have their own priorities.
Some want better tools for patient care, others are focused on improving efficiency, and others are concerned about keeping everything legal. Balancing all these perspectives can be tricky, but involving everyone early on and keeping communication open can help developers create a solution that works for everyone.
Software Development in Healthcare: Best Practices
Getting healthcare software right is about both solid code and making sure it works for the people who rely on it every day. Whether it’s doctors, nurses, or administrators, if the system isn’t intuitive and efficient, it’s going to cause more headaches than help. Here’s how to develop and implement healthcare software that actually makes a difference.
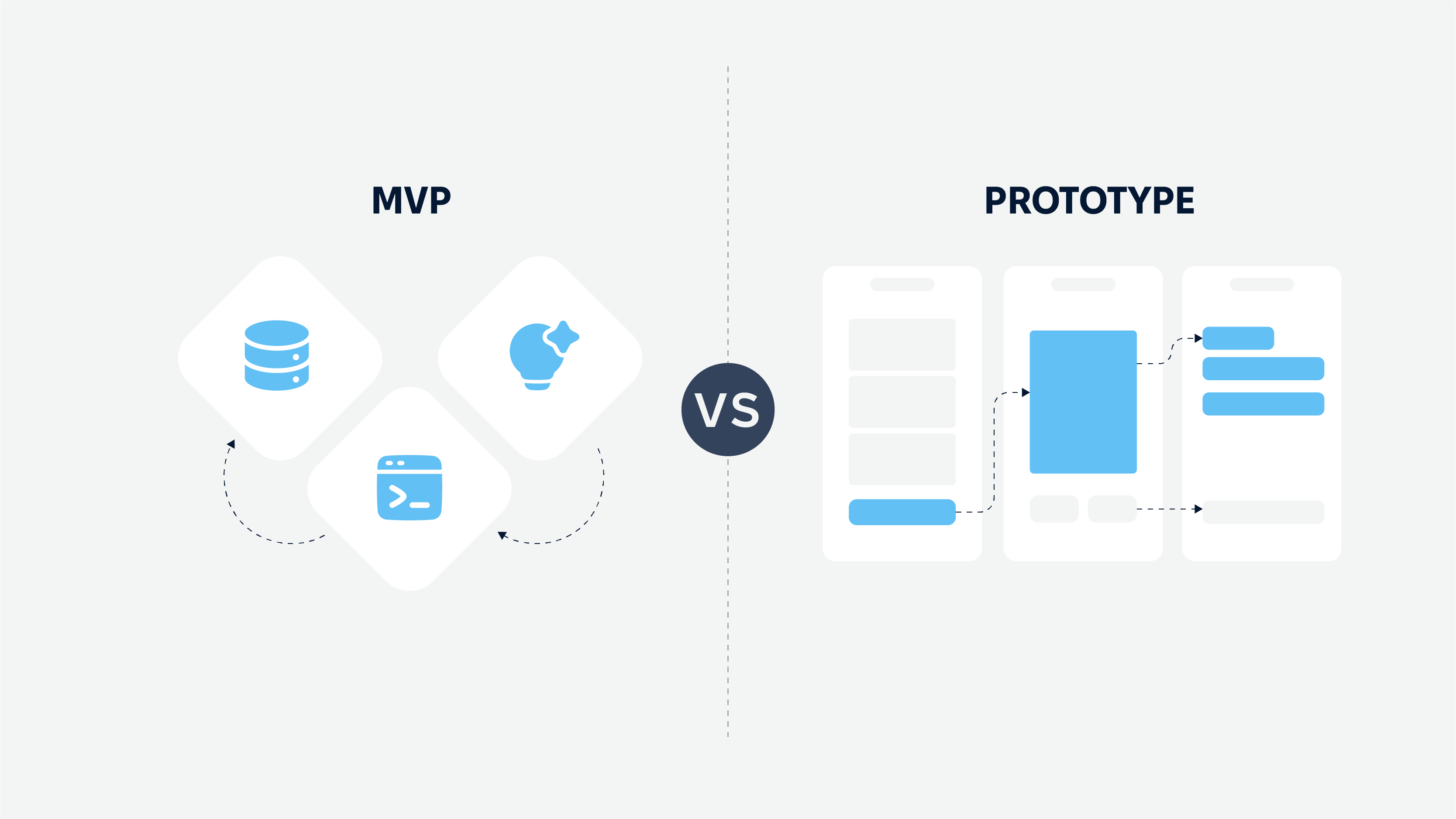
Build in Small Steps, Not Giant Leaps
A successful project starts with an agile approach—think of it like building a bridge while people are already walking across it. Instead of developing everything at once and hoping it works, teams break the project into smaller steps, healthcare software testing, and tweaking along the way.
That’s how a large hospital network fixed its clunky EHR system. Initially, doctors found it time-consuming and frustrating, but by involving them in the design process, developers streamlined the workflow, cutting documentation time by 30% and improving overall satisfaction.
Make Sure Real Users Have a Say
No one knows the daily struggles of healthcare software better than the people using it. A telehealth startup learned this the hard way when their new app launched with major video call issues.
Patients and doctors complained about dropped connections and glitchy interfaces. Instead of waiting for the next big update, the company introduced smaller, frequent fixes based on real-time feedback, improving call stability and overall user experience.
Roll It Out Gradually—And Train People Well
Even the best-designed software can crash and burn if it’s dumped on users too fast. A smarter approach? A phased rollout. A major health system in California tested its new scheduling system in just a few clinics first. That way, they worked out the kinks before rolling it out everywhere—avoiding mass confusion and frustration.
Training also makes a huge difference. When a hospital introduced an AI-powered diagnostic tool, doctors were skeptical. But once they got hands-on training and saw how it helped speed up diagnoses, adoption soared. The takeaway? People don’t trust what they don’t understand.
Change Is Hard—So Manage It Well
People naturally resist change, especially in high-pressure environments like hospitals. When a national healthcare provider replaced its outdated patient portal, users initially pushed back.
However, by addressing concerns early and showing how the new system would save them time, the company turned frustration into acceptance. Clear communication and demonstrating real benefits go a long way in easing the transition.
Keep Improving—Even After Launch
Software development doesn’t stop at launch day. Hospitals using AI-driven analytics now spot workflow bottlenecks and make continuous refinements, improving efficiency and patient care. The best healthcare software isn’t just built—it’s maintained, updated, and optimized over time.
Focusing on real user needs, rolling out software strategically, and staying committed to improvements–all this ensures your tech investments pay off, leading to smoother operations, happier providers, and better patient outcomes.
Success Metrics and ROI
User Adoption Rates
If doctors, nurses, and staff aren’t using the software, it’s not serving its purpose. A smooth, user-friendly interface combined with solid training can make all the difference.
Regular feedback and usability testing help ensure the software works well for everyone, encouraging higher adoption rates. It’s also important to offer continuous support after the initial training. A helpdesk or easy access to resources can give users confidence to navigate the system and make them more likely to stick with it in the long run.
Implementation Timelines
A successful software rollout should be efficient, not drawn out. A clear, structured timeline ensures everything stays on track. Starting with pilot programs or staggered launches can help catch any issues early, making the full implementation process much smoother.
Additionally, being transparent about timelines with your team helps manage expectations and reduce stress. If everyone knows what to expect and when, the transition becomes a team effort rather than a series of surprises.
Cost Efficiency Measures
The right software should save time and reduce costs. Whether by automating routine tasks or minimizing errors, effective software can pay for itself. Tracking improvements, like fewer labor hours or more accurate billing, helps highlight the system’s long-term value.
In addition, it is freeing up time for healthcare staff to focus on what really matters: patient care. The more time they can spend on their core responsibilities, the better the overall outcomes for patients and the organization.
Quality Metrics
Success in healthcare software isn’t just about performance numbers; it’s about real improvements in care. Faster workflows, fewer mistakes, and better patient outcomes are key signs that the software is making a difference.
Regular performance checks and input from clinicians help keep the software aligned with ongoing care improvements. It’s also important to look at patient feedback. When patients notice a difference in their experience—whether it’s easier communication with their doctors or faster appointment scheduling—that’s a clear sign the software is working as it should.
Future Trends in Healthcare Software
AI and Machine Learning
AI is transforming healthcare by making sense of massive amounts of patient data in ways humans simply can’t. From diagnosing diseases earlier to predicting patient deterioration, AI-powered tools are helping providers make better, faster decisions.
For example, AI-driven imaging software is already detecting cancers that radiologists might miss, leading to earlier treatments and better survival rates.
IoT Integration
Wearable devices and smart sensors are making real-time patient monitoring a reality. Hospitals can track post-surgical recovery remotely, while chronic disease patients get continuous updates sent straight to their doctors.
A great example? Smart insulin pens that sync with mobile apps helping diabetes patients manage their condition while giving doctors real-time insights into blood sugar levels.
Predictive Analytics
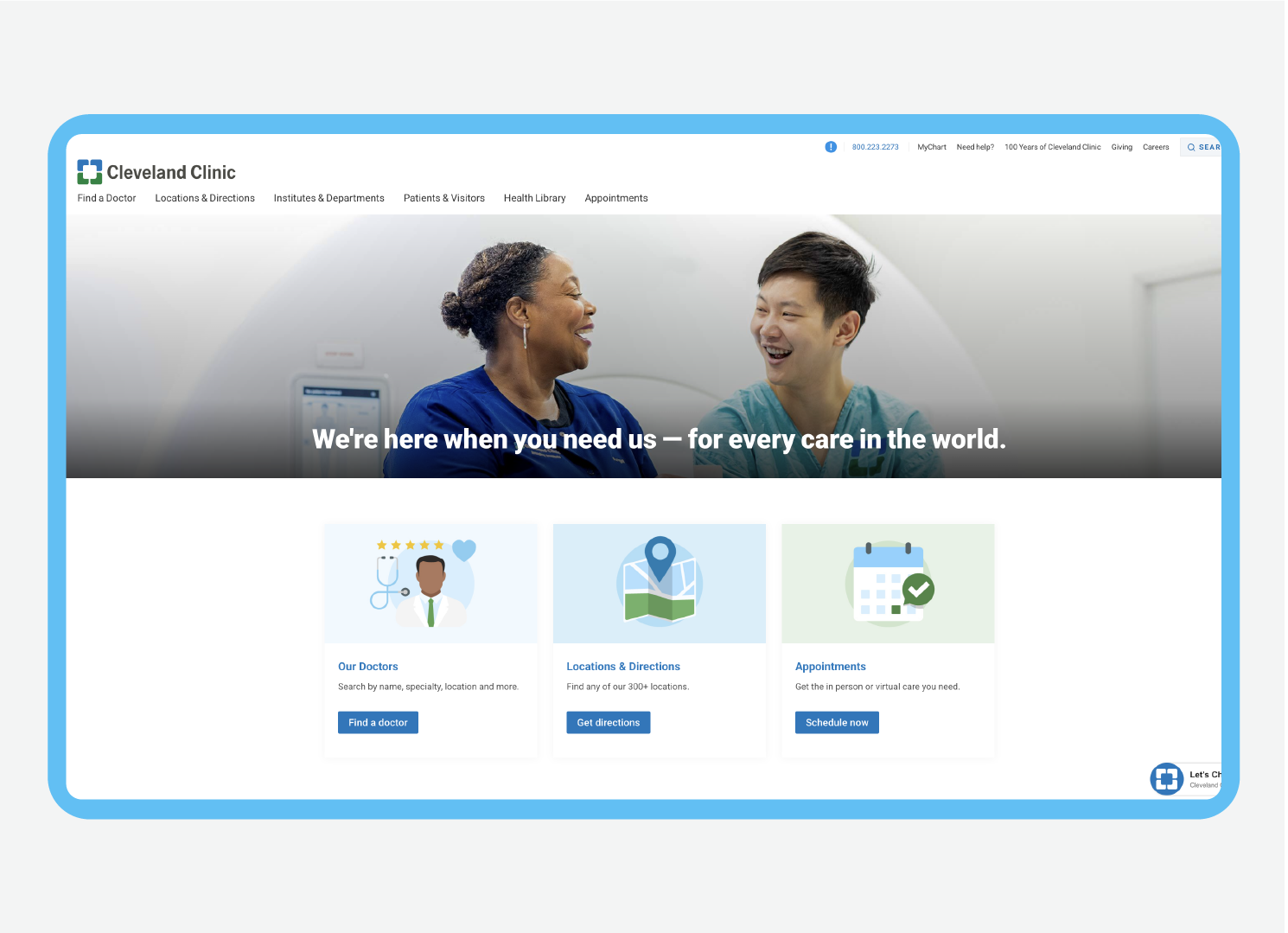
Healthcare isn’t just about treating illness—it’s about stopping it before it starts. Predictive analytics uses past patient data to spot patterns and predict potential health risks. For example, hospitals like the Cleveland Clinic use predictive models to identify patients at risk for heart failure exacerbations. By analyzing patient data, they can intervene early, often preventing serious complications.
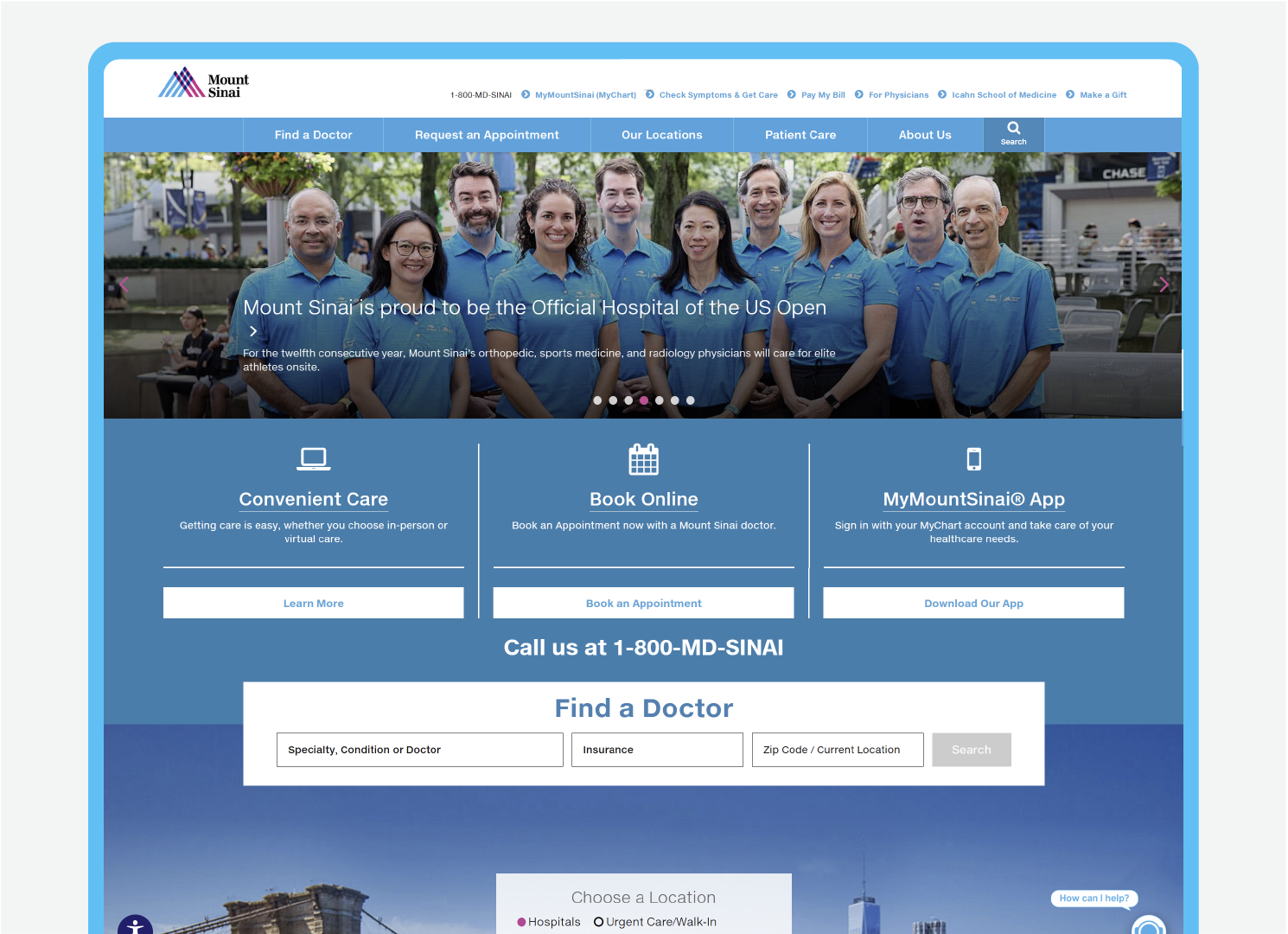
In fact, predictive analytics is already being used to reduce hospital readmissions. For instance, Mount Sinai Health System in New York employs machine learning algorithms to predict which patients are at risk of being readmitted within 30 days of discharge, allowing staff to provide extra care and support before the patient leaves the hospital. This proactive approach not only improves patient outcomes but also helps save costs by avoiding preventable problems.
Mobile-First Development
As healthcare extends beyond the hospital, mobile-friendly software is becoming a must. Providers need to access patient records, test results, and telehealth tools on the go.
The Mayo Clinic, for example, developed its mobile app to give doctors access to patient records and lab results while they’re on rounds or even working remotely. This flexibility allows for better decision-making and faster responses to patient needs. Patients, too, want the flexibility to book appointments, view test results, or connect with doctors from their smartphones.
The MyChart app from Epic Systems is a perfect example of this, letting patients easily schedule appointments, request prescription refills, and communicate with their healthcare providers—all from their phones. Making healthcare more mobile means better care and greater convenience for everyone involved.
Case Studies in Healthcare Software Development
The best way to see the real impact of healthcare software is through real-world success stories. Here’s how Cadabra Studio helped two clients tackle major challenges and made a real difference for both patients and providers.
Remedy Logic: Making Doctor-Patient Communication Easier
Remedy Logic set out to fix a common frustration—how hard it can be for patients to connect with their doctors. They built a telehealth platform that made scheduling appointments, having virtual consultations, and getting prescriptions easier.
By focusing on a simple, mobile-friendly design, they helped reduce missed appointments and made doctors’ days run smoother. The key to their success? Constant feedback from both doctors and patients to fine-tune the platform as they built it.
Read more: Remedy Logic Case Study
Alpha Omega: Helping Hospitals Work Smarter
Hospitals run on a lot of moving parts, and Alpha Omega wanted to make that easier. They developed a system that connected patient records with hospital workflows, giving staff quick access to the information they needed.
The results were huge—fewer documentation mistakes, faster emergency response times, and a system that just made sense for the people using it. Their story proves that when software is designed around real-world needs, everyone benefits.
Read more: Alpha Omega Case Study
Both cases highlight a few key lessons: software should be built with the people using it in mind, rolling it out in phases prevents headaches, and constant feedback leads to lasting improvements. Whether it’s making communication easier or streamlining hospital operations, the right software makes a tangible difference in healthcare efficiency and patient outcomes.
How to Choose a Healthcare Software Development Partner
Choosing a software development partner is like picking the right teammate for a high-stakes game—you need someone who knows the rules, understands the strategy, and can adapt when things get complicated. In healthcare, that means finding a team that not only has top-notch technical skills but also gets the ins and outs of compliance, integrations, and the everyday challenges of providers and patients.
When choosing a partner to build your healthcare software, it’s important to go with one who has experience creating solutions that can grow with you and are easy for your team to use. A great partner will know how to make the software fit smoothly into your existing processes without causing too much disruption.
Keep an eye out for some warning signs. If the partner isn’t clear about how they handle security or doesn’t seem to take data protection seriously, that’s a red flag. You’ll also want someone who knows the ins and outs of healthcare regulations like HIPAA, not just someone guessing their way through the rules.
And be cautious of partners who offer a “one-size-fits-all” solution. Healthcare is complicated, and your software should be built to address the unique needs of your organization. Look for a partner who’s ready to customize their solution for you and offer create from scratch service.
FAQs
What’s the biggest challenge in healthcare software development?
User adoption is often the biggest hurdle. Even the most feature-rich software will fail if it disrupts workflows or frustrates users. Prioritizing usability and seamless integration is key. Engaging healthcare professionals early in the development process can foster better acceptance and smoother transitions.
How long does it take to develop healthcare software?
Development timelines vary based on complexity, but most projects take between six months to two years. Agile methodologies help speed up the process while ensuring continuous improvements. Regular updates and iterations ensure the software evolves with the healthcare industry’s changing needs.
How do I ensure my healthcare software is compliant?
Work with a development team that has deep experience in healthcare regulations like HIPAA, GDPR, and other relevant standards. Regular audits, encryption, and access controls are essential. Additionally, staying updated with the latest regulatory changes ensures your software remains compliant over time.
What types of software are commonly used in healthcare?
Healthcare software includes Electronic Health Records (EHR), telemedicine software, medical billing software, and clinical decision support systems. These tools help healthcare providers manage patient data, streamline operations, and enhance patient care.