In the healthcare industry, data is the heart of everything, starting with making informed decisions and ending with accurate diagnoses and personalized care. In this case, data integration in healthcare is like a tool for solving a puzzle. It takes all the parts and completes the whole picture, making it clear and coherent.
Today, we’ll talk about all the important aspects of healthcare integration, as well as discuss how you can make the most of it.
What is Healthcare Data Integration?
Healthcare data integration resembles constructing a bridge. It collects data from different sources, such as electronic health records (EHRs), medical devices, and even wearable tech, into one unified structure.
Why does it matter? Try to picture a doctor working on a patient’s case without being aware of the patient’s medical history. It is akin to flying with one’s eyes shut!
Data integration makes sure that everything required for patient assistance is available to the concerned person. It automatizes tasks and elevates the overall outcome of patient care. To put it more simply, it is the difference between ‘knowing’ and ‘having a hunch.’
Benefits of Data Integration for Improved Patient Care
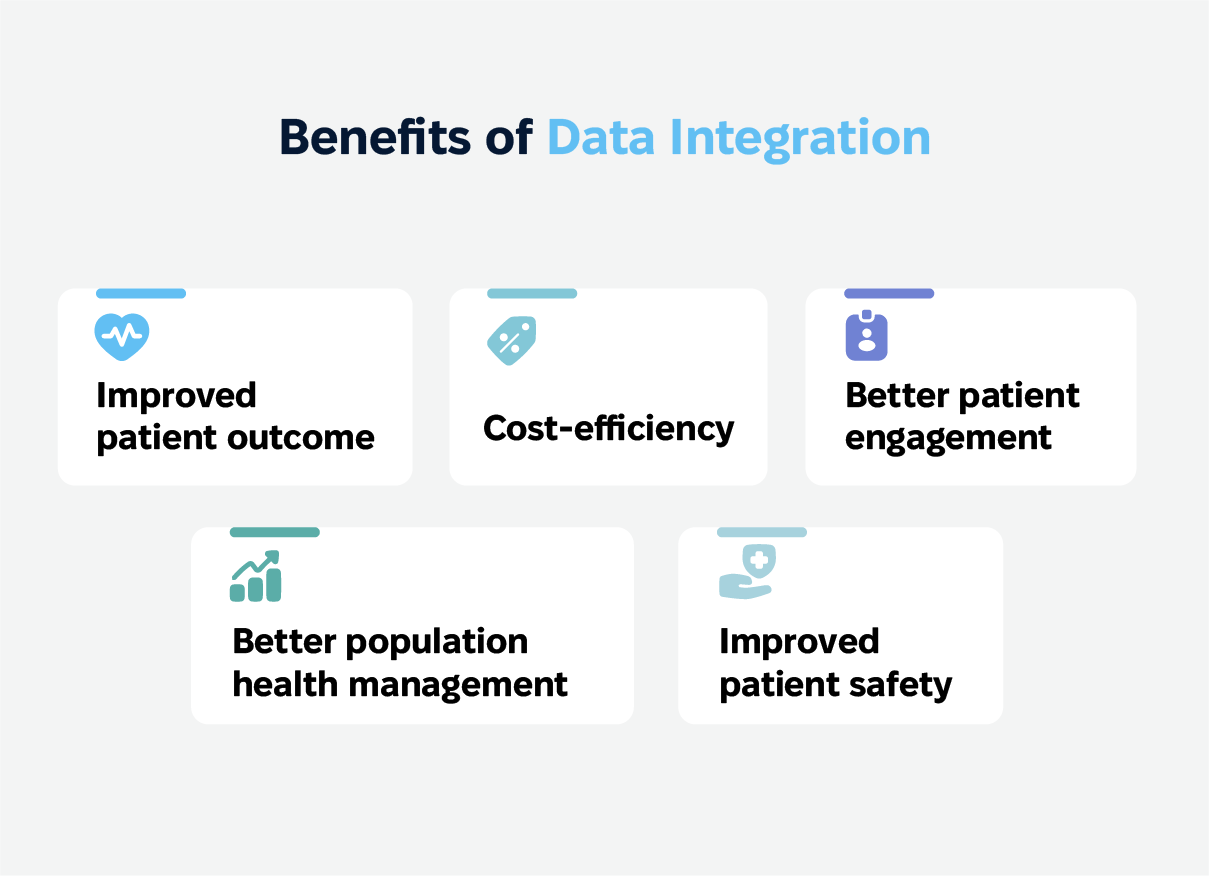
Data integration simplifies processes for doctors, but more importantly, it improves the reach of benefits to patients. Here is how:
Patient outcomes are better. By holding an entire view of a patient’s health, doctors will be able to make informed decisions, such as faster diagnosis and individualized treatments, with immediate access to lab results and the patient’s medical history.
Better engagement with the patient. Patients can check and access their medical records without a hassle, making them engage more in their well-being. It is like giving them the keys to their health journey.
Efficiency increases while costs decrease. Data integration results in more fluent workflows, less manual error, and huge cost reductions. That’s how healthcare systems declutter in shuffling documents.
Better population health management. Translating integrated data into trends and insights allows better management of public health. Risk identification, disease monitoring, etc., can be achieved as well, with integrated health proven to be a great resource.
Improvement in patient safety. The analysis could lead to an alert and monitoring capability for real dangers so that they do not become dangerous actualities, like a safety net for health.
Challenges of Data Integration
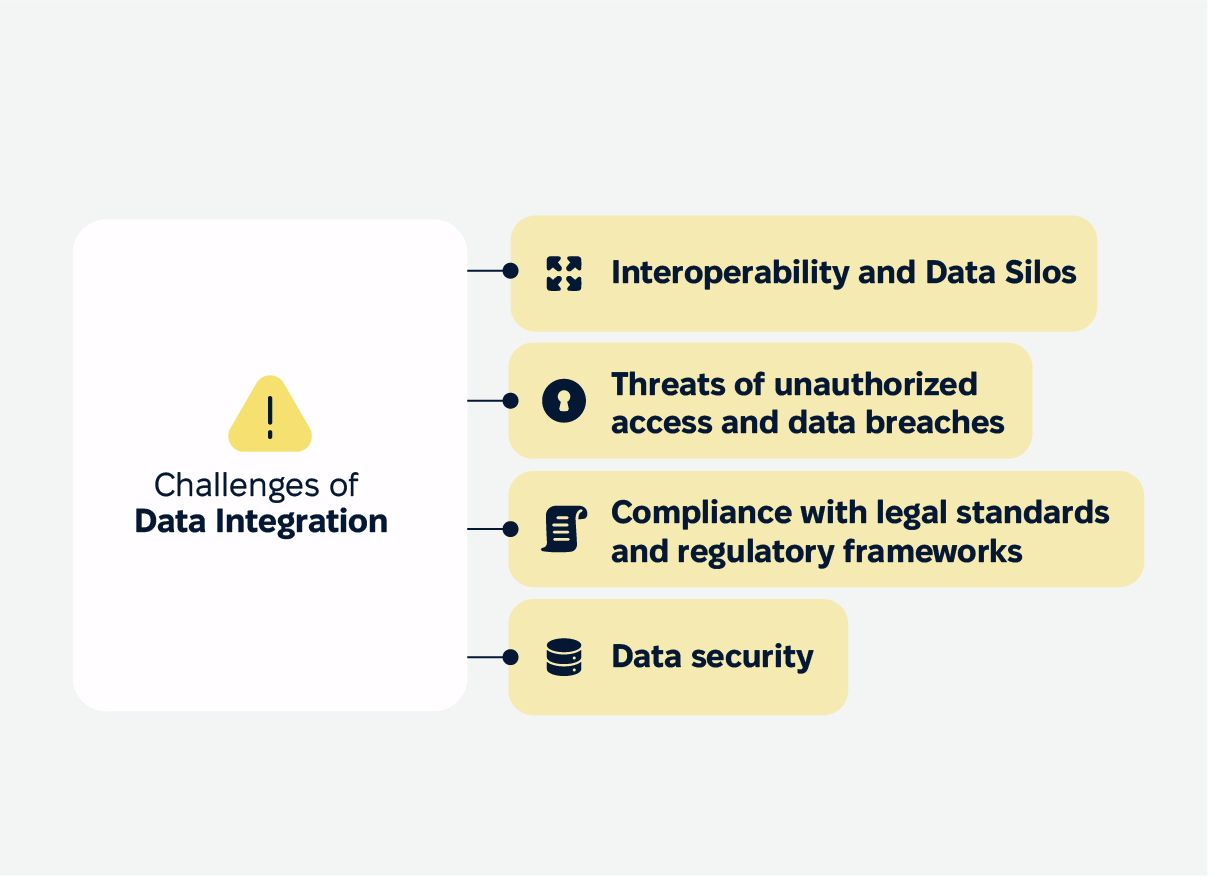
Interoperability and Data Silos in Healthcare Sector
Data silos are created when data is stored in separate systems that do not communicate with each. The lack of interoperability between systems and healthcare providers makes the preposterous task of pushing this data into a shared operational domain much more simplified.
In turn, this results in severe data integration challenges as medical enterprises lack the ability to devise rational and well-thought-out plans that can affect the service being offered to patients. In order to curb these problems, standardization of data is a prerequisite. It serves as the deterrent of the silos and enhances interoperability across the disparate systems.
Data Integration Without Compromising Privacy and Security
Let’s face it: the health information of a patient is too great. Given the growing cyber threats, threats of unauthorized access or data breaches are a medical threat that has become a necessity. This is an aspect that all healthcare units must understand while enabling various systems to integrate this sensitive clinical data.
Further, these legal standards and regulatory frameworks are not only foundational to the legal obligations but also to gaining the confidence and trust of the patients. After all, it is their data. Patients need to be assured that their information is secure. After all, the success and effectiveness of bringing together disparate systems are made possible by good security measures.
Get a free consultation on specific challenges of your organization and how to overcome them.
Regulations for Data Integration and Interoperability
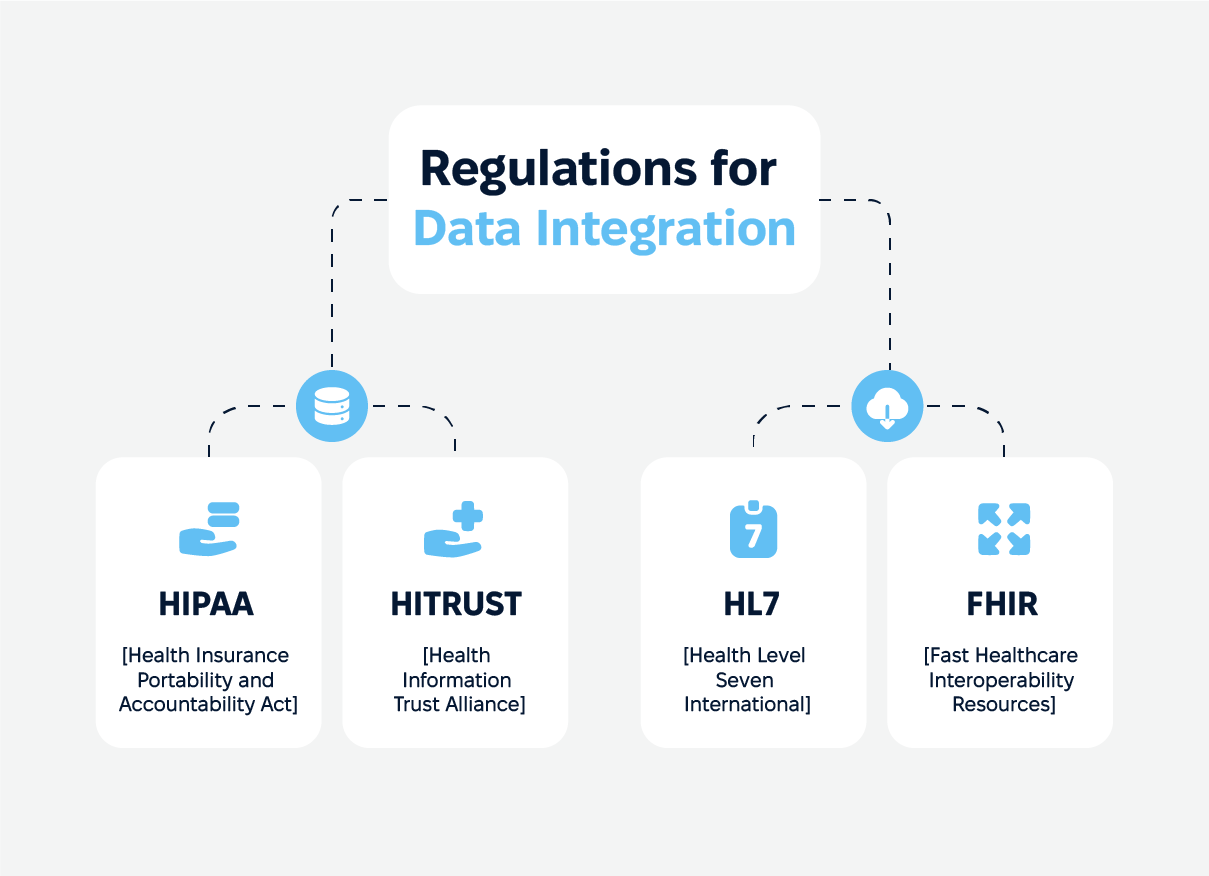
HIPAA and HITRUST Regulations for Healthcare Data
HIPAA (Health Insurance Portability and Accountability Act) regulates the use or disclosure of protected health information (PHI) and requires that these activities be properly addressed.
HITRUST (Health Information Trust Alliance) was created to provide a framework for the management of risks and compliance with HIPAA, which enables organizations to safeguard patient information.
These are mandatory regulations. They must be complied with in order to protect patient information and preserve confidence in the healthcare system.
HL7 and FHIR Standards for Data Exchange
These standards are the glue that holds data integration together:
FHIR (Fast Healthcare Interoperability Resources). This modern standard is aimed at making the exchange of healthcare data electronically quicker and easier to do.
HL7 (Health Level Seven International). A well-known standard used in the industry was created to ensure privacy and security in linkages of clinical and administrative datasets.
Adhering to these standards is essential if you want to share data securely and efficiently and improve collaboration and patient care.
Best Practices for Seamless Data Integration
Know Your Data and Identify Data Sources
Effective data integration begins with truly understanding your data. It’s not just about gathering information but knowing exactly where it comes from and how it’s formatted.
So, healthcare organizations need to identify all the potential sources, like electronic medical records, medical devices, and even wearable tech. Each source has its quirks, so understanding these unique data structures ensures the integration process is more smooth sailing than stormy seas. A solid data governance framework is like the recipe—it keeps everything consistent, high-quality, and on track.
Leverage Cloud-Native Architecture and APIs for Integration
On the technology side, cloud-native architecture is a game-changer. It’s like switching from a bicycle to a high-performance sports car—it’s faster, more flexible, and built to handle the unexpected.
Pair this with APIs (Application Programming Interfaces), which act like expert interpreters, ensuring all your data sources communicate effectively and securely. Together, these tools enable seamless integration, giving healthcare providers the power to deliver better, more efficient patient care. It’s a win-win for everyone involved.
Electronic Health Records (EHRs) in Data Integration
EHRs are the backbone of healthcare data integration. They keep all patient information in one place, making it easy for healthcare providers to access and share data securely.
What makes EHRs so powerful is their ability to provide a comprehensive view of a patient’s medical history. This centralized access empowers healthcare professionals to make well-informed decisions, tailor treatments, and improve overall patient care. In short, EHRs are the unsung heroes that keep the healthcare system running efficiently and effectively.
Data Integration Use Cases in Healthcare
Patient-360 View and Comprehensive Services
A Patient-360 view pulls together data from all corners of a patient’s healthcare journey (medical history, current conditions, medications, lab results, and treatment plans) into one neat package. This gives healthcare providers a full picture of the patient’s health, helping them make smarter, more informed decisions.
For example, Epic Systems does a great job of creating this unified view. It pulls patient data from all departments, including primary care, radiology, lab results, etc., into one record. This gives doctors everything they need to spot care gaps or prevent unnecessary treatments right away.
Crisis Response and Emergency Care
In an emergency, time is everything. That’s where data integration really shines. By having access to real-time, integrated data, healthcare providers can make quick, informed decisions and respond faster, improving care during a crisis.
For instance, NYC Health + Hospitals uses integrated data in their emergency departments to pull in patient records from various sources: previous visits, medications, and diagnostic results. This lets clinicians hit the ground running, making better decisions on care right off the bat.
Data Visualization and Analytics in Healthcare
Data visualization is the best way to present complex information in an easy-to-digest format. It helps professionals make informed decisions that directly improve patient care. From spotting trends in patient outcomes to identifying areas that need attention, visualization tools provide an insightful and practical bird’ s-eye view.
When done right, it doesn’t just highlight what’s happening. It points to why it’s happening and how to address it. It’s a critical tool for any organization aiming to be truly data-driven.
Analytics tools for improved patient outcomes
Analytics tools uncover patterns, identify trends, and solve mysteries hidden within the data. They allow you to dive deep into patient information, providing insights that can significantly improve outcomes.
Analytics tools turn raw data into actionable intelligence, whether predicting potential health risks or tracking the effectiveness of treatments. They’re not just helpful; they’re essential for modern healthcare systems striving to deliver personalized, effective care. With the right analytics tools, providers can stay one step ahead, making proactive, informed decisions that benefit patients and the healthcare system as a whole.
Implementation and Maintenance of Data Integration Solutions
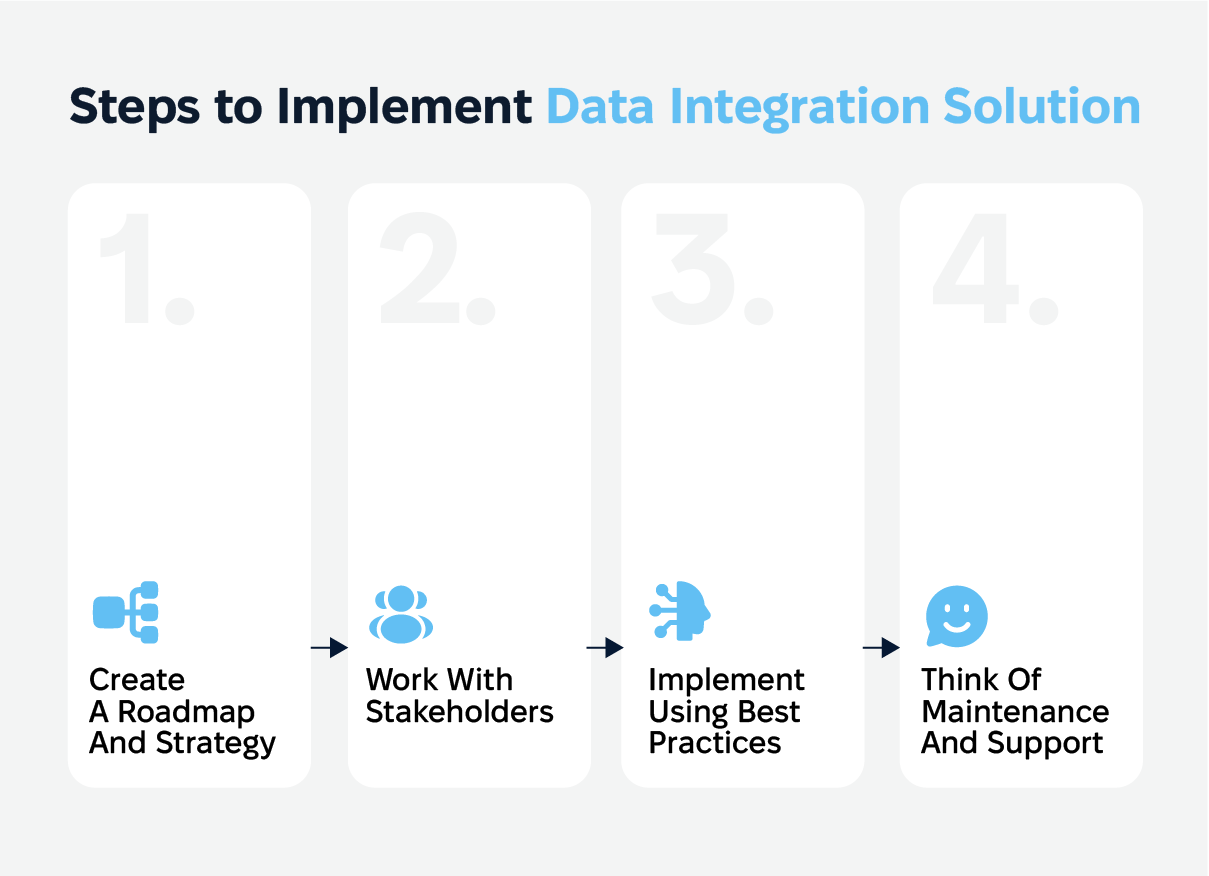
Data integration methods require truly having plans, taking everyone on board, and help and support to ensure effectiveness. Here’s a basic plan which gives some guidance on the work in a more systematic manner.
1. Roadmap & Strategy for Implementation
A mapping strategy is one of, if not the key necessities towards ensuring that the integration process is successful as it outlines procedures to be followed and achievement of goals.
Action steps
Set integration objectives: The integration process should address the need and have clear goals to be achieved ( for example, better care and improved workflows).
Timelines: Specify at what time each critical characteristic must be completed.
Determine allocations: Specify what instruments, finances, and teams are needed to do the work.
2. Stakeholders and Their Roles
Each stakeholder who is required to be fully committed to the process needs to be explicitly stated and their duties defined.
Action steps
Identify interested parties: List teams from IT, project managers, data users, and end users
Define responsibility: Emphasize the role of each stakeholder and what needs to be contributed.
Provide regular updates and discussion: Plan and organize regular meetings for all parties involved.
3. Maintenance Support and Further Enhancement
Once you put into action a data integration solution, you need to periodically maintain the system through support and monitoring to ensure it remains relevant over the years.
Keeping it going
Ensure that your integrated health care has all appropriate upgrades, as well as innovations in technology and security. Furthermore, it is vital to emphasize fixing problems in a timely manner, and therefore, a mechanism for resolving them quickly should be in place. Also, the system should be assessed on an ongoing basis for actual operational capabilities in order to identify opportunities for improvement that will enhance performance.
Training and support
Staff should be fully trained to understand the new system, its features, and the benefits it brings. This will ensure that the users are able to take advantage of the system as intended.
Also, technical support is vital so users can call for a team that addresses any issues from time to time. Making it easy to find documents such as manuals and frequently asked questions would help users to deal with some of the issues with the system on their own thus improving their experience with the system.
Data Governance and Management in Healthcare
A good data governance framework helps keep things organized and consistent. Think of it as a roadmap for how data is collected, stored, shared, and used. To make this work, you need clear rules and policies that spell out who can access the data, how it should be handled, and what everyone’s responsibilities are.
When it comes to managing data, the focus should be on keeping it accurate and intact. This means having strategies in place to avoid mistakes like duplicate or corrupted data. Start by figuring out all the different places your data comes from (like health records, imaging systems, or wearable devices) and get a handle on the formats they’re in. Regular checks and automated tools can help you validate and verify the data to make sure it’s as reliable as possible.
The Future of Health Data: Integrated Data for Integrated Care
The way we handle health data is changing fast, and the future looks promising. With AI and ML, healthcare is becoming data-driven, efficient, and personal. New technologies like cloud-native and APIs are making data sharing easier and more secure. Together, these are the foundations for integrated care, where everything about a patient is connected to improve outcomes.
AI and Machine Learning
AI and ML are changing how we process and analyze healthcare data. These technologies can analyze huge amounts of data—everything from electronic health records to medical images and even genetic information—so doctors can make better decisions faster. For example, AI models have been shown to predict patient outcomes with 76% accuracy, which is a big leap in personal medicine.
By seeing patterns and trends in health data, AI can identify issues before they become problems, providing more proactive care and fewer surprises.
Cloud and APIs
One of the biggest challenges in healthcare today is getting different systems to talk to each other. Enter cloud native and APIs. These technologies allow health data to be shared securely and efficiently across different platforms. With Google’s Cloud Healthcare API, you can integrate data from multiple sources so healthcare providers can get a full picture of a patient’s health.
This kind of data sharing streamlines workflows and ensures that all healthcare providers have access to the right information at the right time so they can make faster, better-informed decisions.
Data Integration in Healthcare Matters
In short, data integration is key to better patient care. When all the data about a patient—medical history, lab results, imaging—is connected, doctors can deliver more personal and effective care. Recent research suggests that better use of healthcare data could lead to better patient outcomes and cost savings.
There are challenges, especially regarding data privacy and fragmentation. To make integrated care a reality, we need to address these issues with good data governance and privacy. But with technology advancing, we’re getting there.
Conclusion
In the healthcare industry, bringing all your data together is a must for providing top-notch, personalized patient care. When different systems work together, doctors can make better decisions, things run smoother, and patients get healthier faster, all while saving money.
However, getting this right isn’t an easy task. It takes the right know-how, smart planning, and solid data security to make it happen. That’s where Cadabra Studio comes in. We’re here to help you tackle these challenges and create data integration solutions that actually work.
Ready to connect the dots and make your healthcare data work smarter, not harder? Contact us, and let’s chat about how we can help you build a better, brighter future for patient care.
FAQs
What is data integration in healthcare?
Data integration in healthcare consolidates information from sources like electronic health records (EHRs) and medical devices into a unified system. This enables healthcare providers to access comprehensive patient information, facilitating informed decisions and enhancing care quality. By integrating data, healthcare systems streamline workflows and ensure relevant patient data is readily available.
How does data integration improve patient care?
Data integration provides healthcare providers with a holistic view of a patient’s medical history and treatment plans, enabling faster diagnoses and personalized care. It enhances communication among healthcare professionals, leading to more coordinated care and improved patient outcomes.
What challenges exist in healthcare data integration?
Challenges include data silos, lack of interoperability, and data privacy concerns. Overcoming these requires strong governance, adherence to standards like FHIR and HL7, and robust security measures to protect data integrity.
How do EHRs aid data integration?
EHRs centralize patient information, allowing secure data access and sharing among healthcare providers. This facilitates informed decision-making and coordinated care by ensuring healthcare professionals have up-to-date patient data.
Why is data privacy crucial?
Data privacy protects sensitive patient information from breaches, maintaining patient trust and compliance with regulations like HIPAA. This trust is essential for effective healthcare delivery and successful integrated health systems.